Summary: A study reveals how brain cell interactions influence aging, showing that rare cell types either accelerate or slow brain aging. Neural stem cells provide a rejuvenating effect on neighboring cells, while T cells drive aging through inflammation. Researchers used advanced AI tools and a spatial single-cell atlas to map cellular interactions across the lifespan
Can AI Enhance PET/MRI Assessment for Extraprostatic Tumor Extension in Patients with PCa?
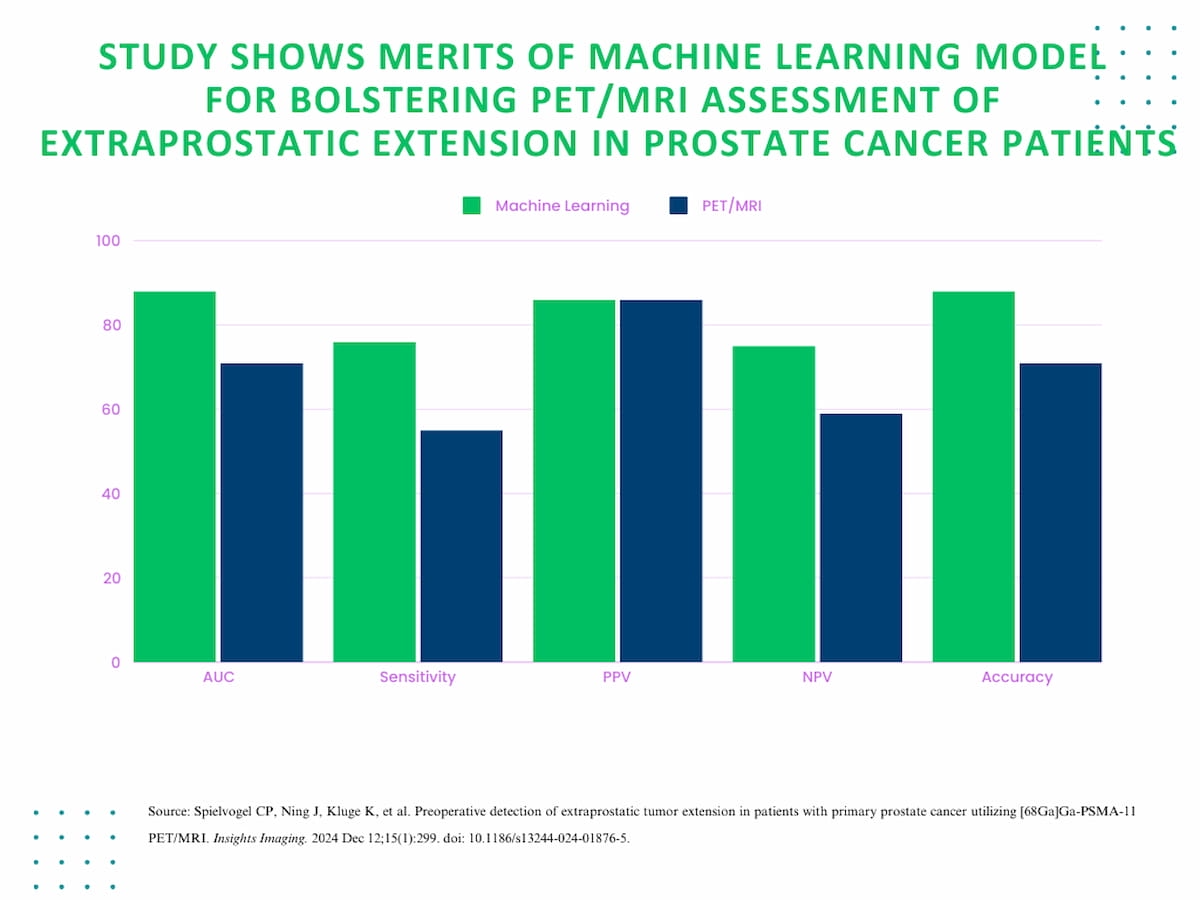
The use of an adjunctive machine learning model led to 17 and 21 percent improvements in the AUC and sensitivity rate, respectively, for PET/MRI in diagnosing extraprostatic tumor extension in patients with primary prostate cancer.
Emerging research suggests that machine learning may significantly enhance the capabilities of positron emission tomography (PET)/magnetic resonance imaging (MRI) for preoperative diagnosis of extraprostatic extension (EPE) in patients with primary prostate cancer (PCa).
For the prospective study, recently published in Insights into Imaging, researchers compared the use of an adjunctive machine learning model to conventional interpretation of (68Ga)Ga-PSMA-11 PET/MRI in 107 patients with primary PCa, 59 of whom had EPE.
The study authors found that the machine learning model had 17 percent higher area under the curve (AUC) and accuracy rates (88 percent vs. 71 percent), and a 21 percent higher sensitivity rate (76 percent vs. 55 percent) in comparison to PET/MRI alone.

For the detection of extraprostatic extension in patients with primary prostate cancer, study authors found that a machine learning model had 17 percent higher area under the curve (AUC) and accuracy rates (88 percent vs. 71 percent), and a 21 percent higher sensitivity rate (76 percent vs. 55 percent) in comparison to PET/MRI alone.

The machine learning model also demonstrated a similar positive predictive value (86 percent) and a lower specificity (82 percent vs. 88 percent), but the researchers also noted a 16 percent higher negative predictive value (75 percent vs. 59 percent).
“(Machine learning) based on routinely acquired clinical data can significantly improve the pre-operative detection of EPE in PCa patients,” wrote study co-author Clemens P. Spielvogel, Ph.D., who is associated with the Department of Biomedical Imaging and Image-Guided Therapy in the Division of Nuclear Medicine at the Medical University of Vienna in Austria, and colleagues.
For Related Content
1. Improved diagnostic accuracy. Machine learning models demonstrated 17 percent higher accuracy (88 percent vs. 71 percent) and sensitivity (76 percent vs. 55 percent) compared to conventional PET/MRI for detecting extraprostatic extension (EPE) in prostate cancer patients.
2. Enhanced predictive performance. The machine learning model showed improved negative predictive value (75 percent vs. 59 percent), indicating better ability to rule out EPE, which is critical for preoperative planning.
3. Clinical relevance for staging and treatment. Integrating machine learning with PET/MRI can enhance TNM staging accuracy, aiding in surgical decisions, radiation therapy, and hormone therapy strategies for prostate cancer management.
For preoperative detection of EPE, the researchers pointed out the challenges of using traditional imaging in isolation, citing the suboptimal sensitivity of multiparametric MRI (mpMRI) and the inability of prostate-specific membrane antigen (PSMA) PET radiotracers to reliably ascertain the surgical extent needed for radical prostatectomies. The study authors said the combination of multimodal imaging and clinical data in machine learning models enhances preoperative EPE assessment.
“Accurate pre-operative identification of EPE is challenging but crucial for the clinical management of PCa patients. EPE, encompassing the tumor’s local spread beyond the prostate, is detrimental for clinical staging and crucial for surgical decision-making, hormone, and radiation therapy decisions. As a consequence, our findings indicate that ML approaches may enhance TNM staging accuracy and treatment decision-making in PCa,” maintained Spielvogel and colleagues.
(Editor’s note: For related content, see “Study Shows PET MRI Offers Better Detection of Localized Prostate Cancer Than mpMRI,” Is PI-RADS Version 2.1 Outdated for Prostate MRI?” and “PSMA PET/CT or mpMRI: Which is Better for Diagnosing Biochemical Recurrence of PCa?”)
In regard to study limitations, the authors conceded possible variations with imaging protocol and scanner use with machine learning models. They also emphasized that additional external validation is necessary to confirm broader applicability of the study findings.