Tech Comments (3) Luis Alvarez Adobe (NASDAQ:ADBE) and GitLab (NASDAQ:GTLB) shares slipped in early trading on Tuesday as investment firm Mizuho said the market believes it is seeing a “severe negative impact” from artificial intelligence. “ADBE sits at the intersection of creative software and generative Quick Insights Recommended For You
Diagnose faster, treat smarter, fight resistance – Oxford Martin School
Diagnose faster, treat smarter, fight resistance

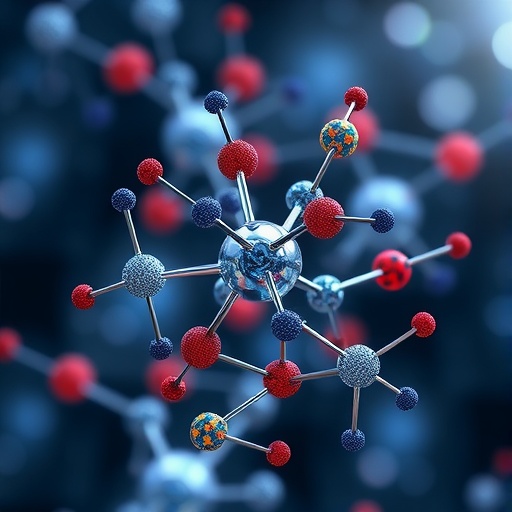
By combining AI, advanced microscopy and engineering the team is revolutionising how infections are diagnosed, and how antibiotics are prescribed.
The Challenge
Antibiotics are becoming less effective. Overuse of broad-spectrum drugs, often due to delays in diagnosis, fuels antimicrobial resistance, already responsible for more than 1.2 million deaths each year. Broad-spectrum drugs continue to be prescribed, however, because current tests to identify bacteria and their antibiotic susceptibility take at least 24 hours, delaying treatment and worsening outcomes. Hence, finding a test that can rapidly identify pathogens and their susceptibility means patients could be treated much faster with narrow-spectrum antibiotics targeting the specific bacteria.
The Approach
The Oxford Martin Programme on Antimicrobial Resistance Testing brings together researchers from physics, engineering and the medical sciences to develop a rapid diagnostic test that delivers results with 30 minutes.

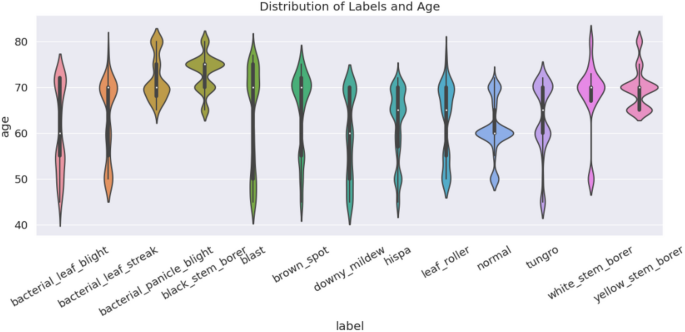
Infection Inspection called on online users to help train AI models to learn what antibiotic-sensitive and antibiotic-resistant bacteria look like under a microscope.
The team also launched Infection Inspection, a global citizen science project to train their AI model, which used over 1 million images which in turn were classified by more than 5,000 volunteers.
The Impact
- 30-minute results: To identify both bacterial species and effective antibiotics – at least 50 times faster than the current standard.
- AI-driven accuracy: Trained deep learning models to distinguish whether bacteria are sensitive or resistant to antibiotics based on visual changes – achieving over 75% accuracy.
- Portable and accessible: Designed for use in hospitals, pharmacies or even field tents serving victims of a natural disaster.
- Targeted treatment. Enables precise, personalised use of narrow-spectrum antibiotics.
What’s Next
The test already works in lab settings and is being refined for speed, offline functionality, and broader antibiotic coverage. The next step is commercial-scale development with the goal of global deployment.
Professor Achillefs Kapanidis, who led the work with colleagues Professor Chris Nellåker, Dr Nicole Stoesser, Monique Andersson and Derrick Crook, explains:
“The average time for bacteria to develop resistance to a new antibiotic is about two years, so they are a very precious resource. In sub-Saharan Africa, east and south-east Asia, and in South America the impact of antimicrobial resistance is already very high, and deaths are predicted to reach 10 million a year by 2050 if we don’t scale up efforts substantially. These new tests will mean doctors can quickly make informed decisions about how best to treat infections. We must prevent the use of broad-spectrum antibiotics to safeguard the future.”